From facility to home: How healthcare could shift by 2025
Up to $265 billion worth of care services for Medicare fee-for-service and Medicare Advantage beneficiaries could shift to the home by 2025.
By Oleg Bestsennyy, Michelle Chmielewski, Anne Koffel, and Amit Shah
How the COVID-19 pandemic has catalyzed Care at Home
A variety of pandemic-related factors have created an opportunity to rethink Care at Home. These include the following:
- Growth in virtual care: In February 2021, the use of telehealth was 38 times higher than prepandemic levels. While the future of reimbursement parity for telehealth is not yet clear, payers and providers have an opportunity to respond to evolving consumer needs. About 40 percent of surveyed consumers said that they expect to continue using telehealth going forward. This represents an increase from 11 percent of consumers using telehealth prior to the COVID-19 pandemic.
- More patients with post-acute and long-term care needs may be evaluating their options: As baby boomers age and families contend with the ongoing impact of the COVID-19 crisis, a growing number of patients and families may be considering their options for post-acute and long-term care. Ideally, eligible individuals would receive care in the most appropriate setting, whether that is at home or in a facility for rehabilitation, assisted living, skilled nursing, or long-term care. A combination of remote monitoring, telehealth, social supports, and home modification may enable more patients to receive some level of Care at Home. The share of Medicare visits conducted through telehealth, for example, rose to 52.7 million in 2020, from approximately 840,000 in 2019, according to a December 2021 report from the US Department of Health & Human Services.3
- Emergence of new technologies and capabilities: New technologies are making Care at Home possible for more people. Remote patient-monitoring devices, for example, allow providers to monitor patient progress remotely and receive alerts if there is an issue. In an April 2021 poll, more than one in five healthcare leaders said that their practice offers remote patient monitoring.4 The pandemic has accelerated the use of remote patient monitoring. For example, the Mayo Clinic used remote patient monitoring for ambulatory management of patients with COVID-19 and found that it was effective, with a 78.9 percent engagement rate; 11.4 percent and 9.4 percent 30-day emergency-department-visit and hospitalization rates, respectively; and a 0.4 percent 30-day mortality rate.5
- Growing investment in the digital health market: Venture funding for digital health companies was a record-breaking $29.1 billion in 2021. Comparatively, there was $14.9 billion invested in 2020 and $8.2 billion invested in 2019.6
Care at Home may deliver more value and higher-quality care
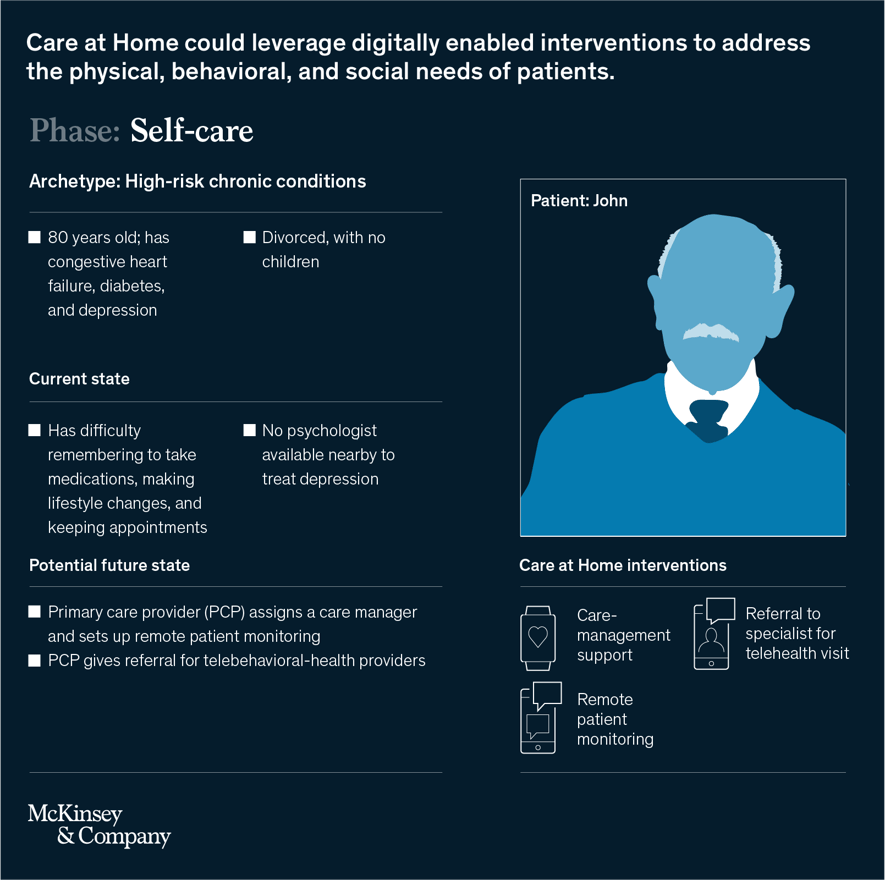
As the United States faces the ongoing COVID-19 crisis, stakeholders are exploring ways to provide higher-quality care, especially for an aging population. The answer may lie with Care at Home, with examples that include primary-care visits via telehealth, self-administered dialysis at home, and skilled nursing-facility services at home with remote patient monitoring and support for activities of daily living. These interventions can be delivered to different kinds of patient archetypes (for example, high-risk patients with chronic conditions or those who are healthy and at low risk) throughout the patient journey (for example, diagnosis, treatment and discharge, or self-care) as either point solutions or as a comprehensive offering.
To examine the current and future impact of this type of care, we have created hypothetical journeys with Care at Home for various patient archetypes (Exhibit 1). For example, consider 75-year-old Bernadette, who has coronary artery disease, chronic obstructive pulmonary disease (COPD), and diabetes. She lives with her husband, has limited mobility, and struggles to access healthy food. Under a traditional-care model, she may be admitted to the hospital with a heart attack and then discharged to a skilled nursing facility because of concerns about her ability to stay safe and engaged at home. Under a Care at Home model, she might be evaluated by a physician and sent home, where she could have an assigned nurse and care manager, remote patient monitoring, daily telehealth visits with a physician coupled with in-person care from a nurse, and meals delivered to her home by a community-based organization.





Where care could shift from traditional facilities to the home
Care at Home cannot succeed without physician buy-in. To understand the percentage of care being delivered in an office or facility today that could be provided at home—in clinically appropriate and cost-effective ways—for different service categories by 2025, we conducted a survey of physicians who serve predominantly Medicare FFS and MA patients.7 We focused on Medicare FFS and MA because beneficiaries expressed an appetite for Care at Home (McKinsey’s Consumer Health Insights survey from June 2021 found that 16 percent of respondents aged 65 and older said that they are more likely now than they were before the pandemic to receive home health services), and some have conditions that could be treated at home at a substantially lower cost. As a result, the opportunity to expand Care at Home services for Medicare FFS and MA beneficiaries could be broader than for other groups.
The survey investigated the extent to which care for a given service can shift to the home in a clinically appropriate and cost-effective way. Based on the results, we estimate that up to $265 billion worth of care currently being delivered in traditional facilities for Medicare FFS and MA beneficiaries (representing up to 25 percent of the total cost of care) could shift to the home. This represents a three- to fourfold increase in the current spend at home for this population today, although how the shift will affect reimbursement rates is not yet clear (Exhibit 3).
We categorized the services that can be delivered at home into three groups:
- Services with capabilities in place that may benefit from scaling: These services include primary care, outpatient-specialist consults, emergency-department and urgent care, hospice, and outpatient mental- and behavioral-health visits. Many of these services have seen an increase in usage during the COVID-19 pandemic.8 These services have the potential to scale at home as point solutions. Our survey results suggest that roughly 15 to 40 percent of additional Medicare FFS and MA spending for these services could be delivered at home, with emergency-department and urgent care on the lower end, at 15 to 20 percent, and outpatient mental- and behavioral-health visits on the higher end, at 30 to 40 percent (Exhibit 4).
- Services where capabilities exist that could be stitched together into a comprehensive offering: These services include dialysis, post-acute care (PAC) and long-term care (LTC), and infusions. Our survey results suggest that roughly 15 to 40 percent of additional Medicare FFS and MA spending on these services could be delivered at home, with dialysis and PAC and LTC on the lower end (15 to 25 percent) and infusions on the higher end (30 to 40 percent).
The capabilities needed to deliver many of these services at home are available today: for example, infusion services of intravenous therapies, post-acute nursing and rehabilitative therapy, and dialysis are already being provided at home, but these services could grow further by bringing together capabilities in a comprehensive offering.9For PAC, such an offering may include a nurse to deliver Care at Home, a remote patient-monitoring device to check patients’ vitals and alert providers if there is a concern, a care manager to follow up with patients to make sure they understand the discharge instructions and to schedule follow-up visits, and prepared meals to be delivered to the home. - Services with some capabilities but others that could be further developed: This category includes a single service: acute care. Our survey results suggest that roughly 20 to 30 percent of additional Medicare FFS and MA spending for acute care can be delivered at home. Some acute-care services can be treated at home today, but others rely on capabilities that require further technological advancement. The Centers for Medicare & Medicaid Services has stated that “treatment for more than 60 different acute conditions, such as asthma, congestive heart failure, pneumonia, and chronic obstructive pulmonary disease (COPD) care, can be treated appropriately and safely in home settings with proper monitoring and treatment protocols.”10 However, higher-acuity and more complicated conditions (for example, severe sepsis, unstable cardiac arrhythmias) cannot yet be treated at home in a high-quality and economical way.
Factors that could affect adoption
The growth of Care at Home services could vary based on several factors. First, stakeholders will need to evaluate which services can be delivered at home to treat patients’ physical, behavioral, and social needs effectively. Care at Home providers, technology companies, and investors could play a role here by accelerating innovation.
Second, adoption could depend on the economic viability of Care at Home. Some healthcare facilities and physician groups have had less incentive to pursue Care at Home for their patients because of the potential for lower (or nonexistent) reimbursement for care if provided at home instead of in a higher-cost setting.11 New reimbursement policies or payment innovation (for example, payment parity for telehealth or value-based payment arrangements) could improve adoption.
Third, physician awareness, perceptions, and capabilities may be factors. Physicians could learn about the capabilities of Care at Home, investigate case studies and results of how high-quality care can be delivered at home, and receive training to administer the interventions. Payers could play an important role in spurring awareness and providing training and education to providers.
Finally, adoption will depend on how patients feel about Care at Home. Patients could be made aware of Care at Home options, and they could state a preference for them over facility-based care. To encourage adoption, payers could cover certain services, and providers could recommend Care at Home to patients where clinically appropriate.
How to accelerate growth
To help accelerate the adoption of Care at Home services, payers, healthcare facilities and physician groups, Care at Home providers, technology companies, and investors could consider a variety of potential actions:
Payers
- Develop a value-backed Care at Home strategy with specific use cases. This may include situations where the reduced medical costs and increased revenues will outweigh reimbursement for services and potential for induced demand.
- Redesign benefits to support direct delivery of Care at Home, as well as enabling services (for example, remote monitoring, care management, social supports, or assistance with daily living).
- Create awareness and provide training and education to providers on the technologies available for Care at Home, as well as their uses and benefits.
- Develop a network of high-value Care at Home providers and technology companies, as well as community-based organizations (for example, food banks), that can support Care at Home.
- Expand reimbursement policies (for example, Care at Home reimbursement at parity with traditional reimbursement) or payment innovation models (such as shared savings on total cost of care) to encourage providers to support Care at Home.
- Adopt utilization-management policies (for example, determination of appropriate discharge destination as part of transition-of-care programs) to facilitate the shift of care to the home from other settings where medically appropriate.
- Leverage care management to raise awareness of Care at Home options with members.
Healthcare facilities and physician groups
- Create value-backed Care at Home strategy with specific use cases in which the economics are favorable and patients benefit from higher-quality and more accessible care.
- Develop Care at Home clinical models to deploy with patients (for example, primary and specialty telehealth care, in-home acute care, or in-home infusion services).
- Establish partnerships with other providers or technology companies that can provide Care at Home or enabling services (for example, remote monitoring, care management, social supports, or assistance with daily living) or build capabilities internally.
- Establish contracts with payers to ensure that Care at Home services are reimbursed in an economically viable way (for example, reimbursement at parity with traditional reimbursement or value-based payment arrangements).
- Develop analytics to identify patients who would benefit from Care at Home based on the use cases (for example, high-risk patients with chronic conditions who could benefit from more support at home to prevent exacerbations).
Care at Home providers, technology companies, and investors
- Develop business cases or investment theses for Care at Home (for example, primary telehealth care, in-home dialysis, and remote monitoring). Size the market potential, evaluate the market landscape, and understand how the market may be evolving.
- Evaluate opportunities, with providers and technology companies assessing how to build, buy, or partner for capabilities, and investors identifying potential assets.
- Implement theses, with providers and technology companies creating new offerings in these markets, and investors investing in assets in the market.










